Cardiovascular Risk
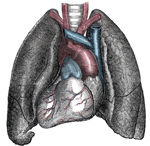 Disordered eating patterns affect the entire body and can result in a variety of serious consequences including an increased cardiovascular risk. Eating disorders are complex conditions that affect a person’s physical, emotional, and psychological well being. All types of eating disorders may negatively impact the cardiovascular system, though the mechanism of damage will vary with the type of abnormal eating behaviors in which a person engages.
Disordered eating patterns affect the entire body and can result in a variety of serious consequences including an increased cardiovascular risk. Eating disorders are complex conditions that affect a person’s physical, emotional, and psychological well being. All types of eating disorders may negatively impact the cardiovascular system, though the mechanism of damage will vary with the type of abnormal eating behaviors in which a person engages.
Rapid Weight Loss Increases Cardiovascular Risk
Rapid weight loss as can occur with Anorexia Nervosa can cause dramatic, unhealthy, and dangerous changes in the heart and sharply increase cardiovascular risk. Anorexia has been associated with mitral valve prolapse, supraventricular and ventricular dysrhythmias, long QT syndrome, bradycardia, orthostatic hypotension, shock, chronic heart failure (CHF), and even sudden cardiovascular death.
These fancy scientific words describe a variety of conditions, but in general, the heart of an Anorexic or person who engages in restrictive eating patterns and experiences significant weight loss, will take a physiologic beating. The heart muscle may be weakened in a variety of ways leading to low blood pressure, an irregular heartbeat, a slow heartbeat, and even sudden death.
Anorexia Can Cause the Heart to Atrophy
The hearts of anorexics will atrophy, meaning that the heart muscle will waste away as the body pulls from even this vital organ to fulfill basic energy requirements. A weakened heart often manifests with bradycardia, a low resting heart rate of less than 50 beats per minute. When the heart is damaged to this extent, caffeine and even exercise can trigger dangerous arrhythmias, or irregular heartbeats. Also, if nutrients are introduced into the system of someone with a heart in this atrophic state, it must be done slowly in order to avoid re-feeding syndrome which can increase cardiovascular risk for arrhythmias, tachycardia (fast heart rate), CHF, and sudden cardiac death.
Bulimia also Associated with Cardiovascular Risk
Bulimia can also increase cardiovascular risk. Purging behaviors can lead to both dehydration and electrolyte imbalances. Sodium and potassium may become depleted to the point that the heart cannot beat properly. Low phosphate and low magnesium may also compound the problem. Both oral and rectal evacuations can cause severe electrolyte and metabolic derangements that can lead to dangerous heart dysrhythmias and even heart attack and death.
A person doesn’t have to be diagnosed with Anorexia Nervosa or Bulimia to experience cardiovascular risk. A person diagnosed with an Eating Disorder Not Otherwise Specified (EDNOS) or who engages in any disordered eating behaviors on the spectrum of eating disorders such as fasting, excessive exercise, starvation, binging, or purging can experience the same risks as those diagnosed with a specific disorder.
Binge Eating Disorder and Cardiovascular Risk
In addition, people with Binge Eating Disorder (BED) can also be at increased cardiovascular risk, especially if they are overweight or obese. People who have been diagnosed with BED have increased cholesterol levels and higher blood pressure as compared to controls. Both high cholesterol and high blood pressure increase cardiovascular risk for both heart attack and stroke. In addition, people with BED or other overeating disorders may be an increased risk for developing Type 2 Diabetes, which if present, is an independent cardiovascular risk factor.
Whether a person is denying themselves proper nutrients or overindulging in them, all disordered eating behaviors can increase cardiovascular risk. Cardiovascular risks associated with eating disorders such as Anorexia Nervosa, Bulimia, and BED can be sudden or severe. Comprehensive treatment for any eating disorder should encompass a holistic approach, including assessing, monitoring, and, as necessary, intervening upon, any present cardiovascular risk.
Eating disorders are also associated with osteoporosis.
 Eating Disorder Self Test. Take the EAT-26 self test to see if you might have eating disorder symptoms that might require professional evaluation. All answers are confidential.
Eating Disorder Self Test. Take the EAT-26 self test to see if you might have eating disorder symptoms that might require professional evaluation. All answers are confidential.